A 14-year-old boy from Kozhikode, Kerala, lost his life to a brain-eating amoeba on Wednesday. The boy, identified as EP Mridul, had been battling an infection known as amoebic meningoencephalitis, a rare and often fatal condition. This tragic incident marks the third such death in Kerala within the past three months.
Table of Contents
The Infection and Its Deadly Toll
Amoebic meningoencephalitis is caused by a free-living amoeba found in contaminated water. This infection is particularly rare but extremely severe, often resulting in death. Mridul, a student at Farook Higher Secondary School, had been admitted to a private hospital last week with symptoms including vomiting and headache. Despite immediate medical intervention, he succumbed to the infection on July 3 at 11:20 pm.
The Source of Infection
Mridul had reportedly bathed in a pond, which health officials later advised the public to avoid. They also warned others who had recently used the pond to be vigilant for symptoms of the infection. This case follows the deaths of two other children from the Malappuram and Kannur districts earlier this year, both of whom also contracted amoebic meningoencephalitis.
Understanding Amoebic Meningoencephalitis
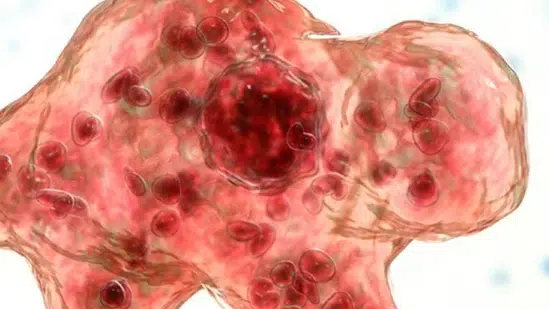
Amoebic meningoencephalitis is primarily caused by the amoebae species Naegleria fowleri and Acanthamoeba. These organisms, often referred to as “brain-eating amoebas,” infect people through contaminated freshwater. The amoeba enters the body through the nose, then migrates to the brain, where it feeds on nerve tissue and causes severe inflammation. Symptoms typically begin 1-9 days after exposure and include headache, fever, nausea, vomiting, stiff neck, seizures, altered mental status, and hallucinations. The disease progresses rapidly and can result in death within 1-12 days of symptom onset.
Health Authorities on High Alert
In response to these incidents, health authorities have urged the public to exercise caution when swimming in potentially contaminated water sources. The infection is not transmitted from person to person and cannot be contracted by drinking contaminated water. However, the risk of infection remains significant, especially in warm freshwater environments. Previous cases of this infection have been reported in the coastal Alappuzha district in 2017 and 2023.
The Challenge of Treatment
Treating amoebic meningoencephalitis remains a significant challenge. There are no definitive treatments, and the disease has a high mortality rate. Doctors typically use a combination of drugs, including amphotericin B, azithromycin, fluconazole, rifampin, miltefosine, and dexamethasone. However, these treatments have not been consistently effective. The US Centers for Disease Control and Prevention (CDC) notes that most individuals with primary amoebic meningoencephalitis die within 1 to 18 days after symptoms begin, often leading to coma and death within about five days.
Recent Cases and Precautionary Measures
The death of Mridul is a stark reminder of the dangers posed by this rare infection. On May 20, a five-year-old girl from Munniyoor in Malappuram also died from primary amoebic meningoencephalitis after bathing in a local river. Additionally, a 12-year-old boy from Ramanattukara, Malappuram, is currently in critical condition at Baby Memorial Hospital after developing symptoms such as fever, headache, and vomiting within 5-6 days of swimming in a pond.
Health authorities continue to monitor and take preventive measures to protect the public from this deadly amoeba. Public awareness and caution are crucial in preventing further tragedies caused by amoebic meningoencephalitis.